The IVF Process includes multiple steps
At Park Avenue Fertility, we use advanced fertility treatment such as IVF to give our patients the best odds for success. For many, the IVF process results in the birth of a long-awaited baby. However, the IVF process can be overwhelming. At Park Avenue Fertility, we walk you through each step of the process. We want you to be comfortable and knowledgeable about the process you have chosen to undertake.
What are the steps of the IVF Process?
Below, we explain each step of the IVF process. During your visits at our Connecticut fertility clinic we will explain each step before and during the process.
Step 1: Ovarian stimulation
Treatment cycles are typically started on the third day of menstruation and consist of a regimen of fertility medications to stimulate the development of multiple follicles (that contain eggs) of the ovaries. Patient usually first start birth control pills to “rest” the ovaries prior to taking stimulatory medications. Shortly thereafter, patients start taking injectable fertility medications (containing follicle stimulating hormone, FSH and/or luteinizing hormone, LH, and are subsequently closely monitored. Monitoring is accomplished by both blood work (to check hormone levels) and by ultrasound (to monitor the growth of the follicles that contain the eggs). Approximately 10-12 days of stimulatory injections are needed to achieve optimal follicular growth and development.
Step 2: Egg (oocyte) retrieval
When egg maturation is judged to be adequate by ultrasound and blood work, human chorionic gonadotropin (hCG) is administered by injection. hCG matures the eggs prior to removing them from the ovaries; this last injection is needed to ensure that all eggs retrieved are mature and capable of being fertilized. The eggs are retrieved from the patient transvaginally. Using ultrasound guidance, a needle is carefully introduced through the vaginal wall and into the ovaries. Gentle suction is applied, and the fluid from each ovarian follicle is removed, along with the egg.
This fluid (with the eggs) is transferred to the embryologist in the IVF laboratory, who then identifies the eggs and transfers them to incubators. The egg retrieval procedure takes about 15-20 minutes and is performed under local anesthesia and light sedation.
Step 3: The in vitro fertilization laboratory
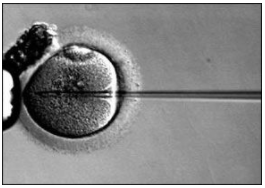
In our IVF laboratory, the eggs are stripped of surrounding cells (which initially are there to support the growth of the egg) and prepared for fertilization. In the meantime, semen provided by the male partner (or a donor) is prepared for fertilization by removing inactive cells and seminal fluid, thus isolating healthy, motile (moving) sperm. The sperm and the egg are then incubated together (about 75,000 – 100,000 sperm are incubated with each egg) in the culture media (a neutral solution similar to that found in the fallopian tube) for approximately 18 hours. In situations where the sperm count is too low to place thousands of sperm with the egg, a single sperm is injected directly into the egg by a technique called intracytoplasmic sperm injection (ICSI). With ICSI, if there are ten eggs, then only a total of ten healthy sperm are needed to achieve fertilization. Fertilized eggs are now termed embryos.
|
|
|
Historically, embryos were transferred three days after retrieval. Now, almost all embryos are transferred five days after retrieval. A five day embryo is called a blastocyst, and it contains over 200 cells.
Step 4: Embryo transfer
The highest quality embryos are then transferred to the patient’s uterus using a thin, soft catheter which is passed through the cervix and into the uterus. This is performed by speculum exam. No anesthesia is needed at the time of embryo transfer. Usually, one embryo is transferred. In some instances (based on a patient’s age and history), more than one embryo may be recommended for transfer. Immediately after the embryo transfer, the patient lies down for approximately 20 minutes before being discharged home.
Step 5: Post-transfer
A pregnancy test is checked 14 days after the egg retrieval (14 days from when fertilization occurred, which corresponds to 9 days after the embryo transfer). During this time period, patients take progesterone—a hormone that maintains the uterine lining and helps to make it suitable for implantation – either by injection or by vaginal suppository. If a patient becomes pregnant, she continues progesterone supplementation through 8-10 weeks of pregnancy.
Women undergoing in vitro fertilization must take some form of progesterone supplementation, since both the medications during stimulation and the egg retrieval procedure itself prevent her body from making adequate amounts of progesterone. Pregnancy rates from IVF vary – they are dependent upon the patient’s age, reproductive history, and diagnosis. In general, younger patients have a higher rate of success from in vitro fertilization compared to older patients. Rates of success are also determined by the quality of the eggs and sperm and resultant embryo quality.
Once pregnancy is achieved, the chances of having a live birth are the same as that compared to a pregnancy achieved in a spontaneous pregnancy. Pregnancies achieved from in vitro fertilization are not considered to be high-risk. Miscarriage rates are similar to that observed among patients who conceived without undergoing IVF.
The IVF process enables patients to bypass fertility challenges
Please contact us if you’d like to learn more about the IVF process and whether it can help you welcome a baby. Our team is here to help you on your path to parenthood.
Contact Us for More Information